Introduction: Daratumumab (Dara) has changed the treatment paradigm in newly diagnosed and relapsed AL amyloidosis (RAL). Efficacy of Dara retreatment in RAL and Dara reexposure with (w/) effective partners such as IMiDs is unknown. We hypothesize that DPd [Dara, pomalidomide (Pom) and dexamethasone (dex)] in previously Dara exposed RAL patients (pts), including pts with low dFLC (20-50 mg/L), will yield deeper hematologic (hem) responses.
Primary objective is to determine hem best response w/in 12 months (mos) of DPd treatment. Secondary objectives include hem overall and very good partial response rates (ORR and VGPR), stringent dFLC response, low-dFLC PR rates (in low dFLC pts only), minimal residual disease (MRD) negative rates using next generation sequencing (NGS), serum mass spectrometry (MS) M protein detection, time to first/ best hem responses, time to next therapy, median hem PFS/OS, organ response rates and duration of/ time to organ response.
Methods: Multicenter phase 2 trial w/16 pts planned to receive DPd for 12 cycles. Eligibility include RAL, ≥ 1 prior line, ≥ 8 prior doses of Dara given in any prior line and negative CRAB criteria. Low dFLC pts were eligible w/ adapted response criteria used for low-dFLC PR (dFLC <10mg/L). Pts received DPd x 12 cycles with optional continuation of Dara and/or Pom w/ or w/out dex per MD discretion if ≥ VGPR achieved after 12 cycles (C). Dara 1800mg SQ weekly (qwk) x 8, every 2 wk X 8 doses & monthly starting C7; Pom 4mg PO Days(D)1-21/28; dex C1: 20mg IV D1/8, 20mg PO D2/9 & 40mg PO C1D15 wkly through C6, then 20mg IV monthly starting C7D1 & 20mg PO D8,15, 22. A reduced starting dose of dex 20mg was allowed for significant cardiac and/or renal disease. Serum MS and NGS from bone marrow were collected at baseline, best response, after 12 cycles, and at 18 and 24 mos follow-up. All pts gave written IRB-approved informed consent.
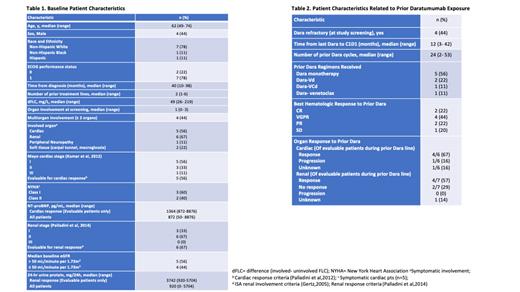
Results: Between 3/2021- 6/2023, 9 pts were enrolled, including 5 w/ low dFLC. Tables 1& 2 show baseline pt characteristics. Five pts completed all 12 cycles (2 w/ measurable dFLC at enrollment and 3 w/ low dFLC); 3 of 5 remain on therapy beyond 12 cycles [DPd (1 pt) & Pom (2)]. An additional 3 pts have completed 1, 5 and 6 cycles of DPd and receive ongoing therapy. One heavily pretreated pt w/ 6 prior lines w/o response (NR) after C2 came off study due to worsening preexisting peripheral neuropathy (PN) and a treatment-emergent grade 3 PN. Of the 5 pts evaluable for response, both measurable dFLC pts achieved CR and negative serum MS; time to best response was 3 and 4 mos. Two of the 3 low dFLC pts (67%) achieved low-dFLC PR; the other had NR despite a decreasing dFLC which started rising w/in 2- 5 mos off therapy. All 3 pts who continue on study therapy past 12 cycles have sustained hem and renal responses at 12, 18 & 26 mos from treatment start. Of the pts on active therapy who have received 1, 5 and 6 cycles to date, 2 achieved VGPR after 1 and 2 cycles, and 1 low dFLC pt achieved low-dFLC PR after 1 cycle. 67% (6/9) and 56% (5/9) are evaluable for renal and cardiac responses, resp. 83% (5/6) achieved renal responses in a median of 2 cycles and cardiac response was seen in 20% (1/5) after 1 cycle (a low dFLC pt). Only 1 renal progression at 14 mos was seen in a low dFLC pt who had therapy held after 12 cycles. This pt also had a renal response after 1 cycle which was sustained through 24 mos. 40% of evaluable cardiac pts (2/5) had cardiac progression after 1 and 2 cycles, resp. All pts remain alive.
DPd was well tolerated w/ expected adverse events (AEs), mostly grade (gr) 1/2 cytopenias and dex related AEs. Gr 3/4 neutropenia in 2 pts was associated w/ gr 1/2 infections only (1 pt w/ suspected undiagnosed benign familial neutropenia (Duffy null phenotype). Both pts continued Pom reduced from 4mg to 2mg on study. Gr 3 non-hem AEs included 2 pts w/ respiratory infections (both w/ gr 1/2 neutropenia) and a pt w/ pulmonary emboli after air travel who was started on apixaban. All pts had full recovery and remained on study therapy. There were no gr 4 infections/ non-hem AEs or discontinuations due to TEAEs other than the previously described gr 3 PN.
Conclusions: We show evidence of safety and efficacy of DPd in previously Dara exposed RAL among the first 5 evaluable pts completing 12 cycles. Hem responses were early and deep in measurable dFLC (CR 100%) and low dFLC (PR 67%) cohorts. An 83% renal response rate occurred early (median 2 cycles). The study is ongoing and updated outcomes including MRD analyses will be presented at the meeting.
OffLabel Disclosure:
Rosenbaum:Janssen Pharmaceuticals: Research Funding. Liedtke:Allogene: Other: Grants or contracts; BMS: Other: Grants or contracts; Participation on a Data Safety Monitoring Board or Advisory Board; Caelum: Other: Grants or contracts; Adaptive: Other: Participation on a Data Safety Monitoring Board or Advisory Board; Abbvie: Other: Grants or contracts; Seagen: Other: Grants or contracts; Janssen: Other: Grants or contracts; Participation on a Data Safety Monitoring Board or Advisory Board; Kite: Other: Participation on a Data Safety Monitoring Board or Advisory Board. Sloan:Nuvectis Pharaceuticals: Consultancy; Stemline Pharmaceuticals: Consultancy; Servier Pharmaceuticals: Honoraria; Seagen: Research Funding; CTI Biopharma: Honoraria; Abbvie: Consultancy. Sanchorawala:Janssen, Alexion, Prothena, Celgene, Takeda, Abbvie, Regeneron, Pfizer, AstraZeneca: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. D'Souza:Abbvie, Sanofi, Takeda, TeneoBio, Caelum, Prothena: Research Funding; Janssen, Prothena: Consultancy; Imbrium, Pfizer, Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees.
Pomalidomide (considered off-label in systemic light chain amyloidosis) but supported by peer reviewed literature for relevant off-label use in this disease as an active drug.